You know that feeling when you wake up and your knees are stiff, or your fingers don’t bend quite right first thing in the morning. For millions of people worldwide, that’s not just a temporary inconvenience it’s their daily reality. Arthritis affects roughly 100 million people globally, and if you or someone you love deals with joint pain, you’re not alone in this struggle.
Here’s the thing about arthritis that doesn’t always get mentioned: it’s not just about old age. While it’s true that arthritis becomes more common as we get older, young people get it too. Athletes, people with certain autoimmune conditions, and even those who’ve had previous injuries can develop arthritis at any point in their lives.
What Actually Happens Inside Your Joints
Your Joints Are More Complex Than You Think:
Let’s start with the basics, because understanding how your joints work makes everything else make sense. Your joints aren’t just the creaky parts of your body they’re actually pretty sophisticated biological structures. Think of them as the hinges that let your body move. But unlike a door hinge, your joints are covered with a slippery substance called cartilage, which helps everything glide smoothly together.
When everything’s working properly, this setup is remarkable. Your knee joint alone handles forces several times your body weight with every step you take. Your hands perform intricate movements thousands of times a day without you even thinking about it. But when arthritis enters the picture, something goes wrong in this carefully balanced system.
The Role of Cartilage and Inflammation:
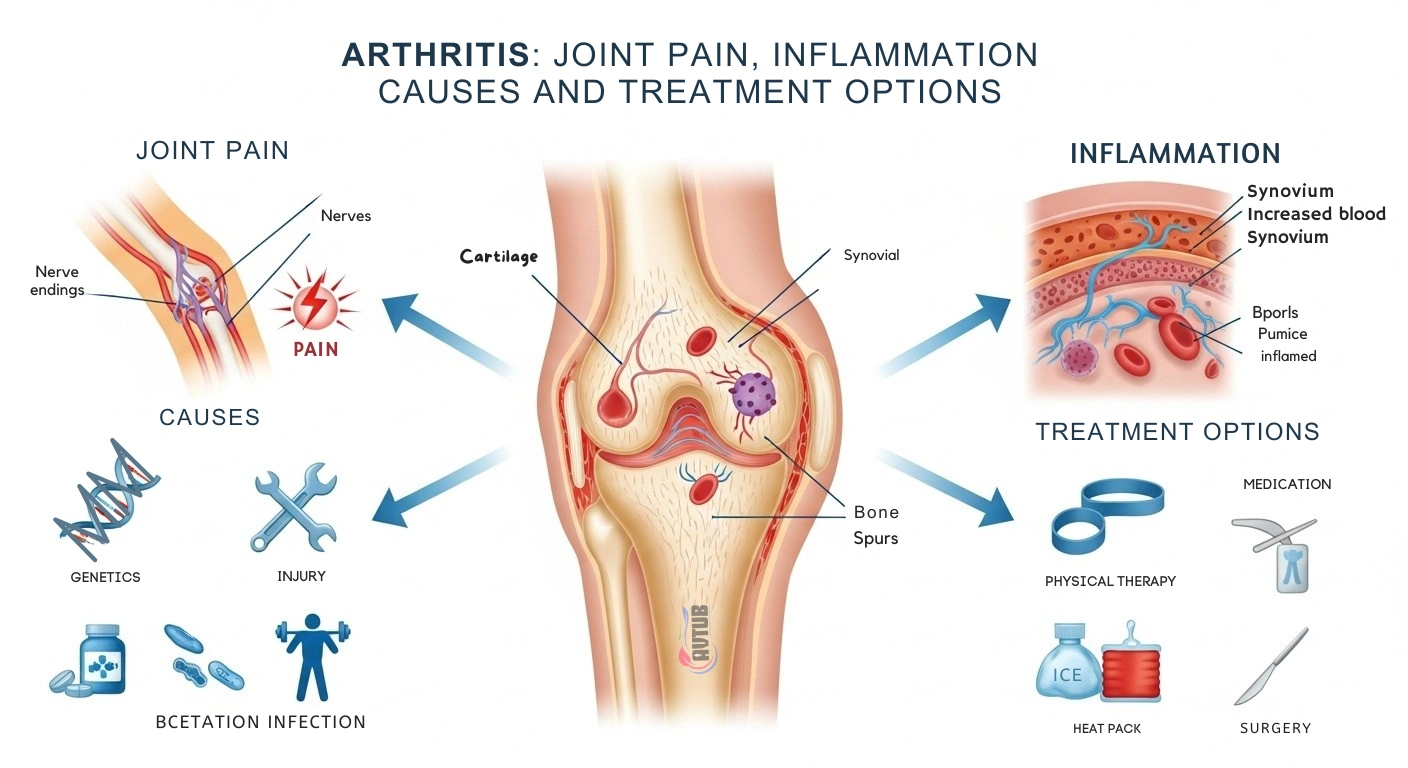
Here’s where cartilage comes into play. It’s kind of like the protective padding in your joints smooth, rubbery, and designed to absorb shock and allow movement without friction. Surrounding your joints is a membrane that produces fluid (called synovial fluid) that keeps everything lubricated and nourished. When you have arthritis, your immune system or wear and tear starts attacking this protective system.
Inflammation that’s the body’s response to injury or threat becomes the enemy in arthritis. Your immune system cranks up the inflammation, which causes swelling, redness, warmth, and pain. In some cases, this inflammation actually damages the cartilage itself, breaking it down faster than your body can repair it. It’s like your immune system is overreacting to a threat, but the real damage ends up affecting you.
Why Understanding Inflammation Matters for Treatment:
Inflammation isn’t inherently bad. Your body needs it to fight infections and heal injuries. But when inflammation becomes chronic when it sticks around for weeks, months, or years that’s when it becomes problematic. Chronic inflammation in your joints leads to persistent pain, limited movement, and progressive damage that makes simple tasks increasingly difficult.
This is why so many arthritis treatments focus on reducing inflammation. It’s not just about feeling better in the moment; it’s about slowing down the damage happening inside your joints. When you understand this, you start to see why some treatments work and others don’t. You’re not just treating pain you’re trying to calm down an overactive immune system or prevent further deterioration.
The Different Faces of Arthritis Types and How They Differ
Osteoarthritis: The Wear and Tear Culprit:
Osteoarthritis (OA) is the most common type of arthritis, affecting millions of people. Think of it as wear and tear on your joints. Over time, the cartilage that protects your bones gradually breaks down. This usually happens because of age, repetitive stress on joints, previous injuries, or just the way your body is built.
If you’ve had a sports injury or accident that damaged a joint, that joint is more likely to develop osteoarthritis down the line. Athletes, people in physically demanding jobs, and those who’ve had broken bones in their joints are at higher risk. It’s not that osteoarthritis is punishment for being active it’s just that joints that have been damaged once are more vulnerable to deterioration later.
The progression of OA is usually gradual. You might notice a little stiffness in your knee after a long day, or your hands ache more when you’re doing repetitive motions. Over time, these symptoms can get worse. The good news? OA progresses slowly in many people, and treatments can significantly slow its progression and improve how you feel.
Rheumatoid Arthritis: When Your Immune System Misfires:
Now we get into the autoimmune conditions, and rheumatoid arthritis (RA) is the most common one. Here’s what’s happening: your immune system is confused. Instead of attacking viruses and bacteria like it’s supposed to, it starts attacking the lining of your joints. This is called the synovial membrane, and when your immune system attacks it, you get serious inflammation.
RA is different from OA in a crucial way. It’s not just about wear and tear it’s your body attacking itself. This is why RA can develop suddenly, often hitting multiple joints at once. Someone might wake up one morning with swollen, painful hands, shoulders, and knees. It affects younger people more often than OA does, though it can develop at any age.
The tricky part about RA is that it’s systemic, meaning it affects your whole body, not just your joints. Some people with RA experience fatigue, fever, and general malaise. If left untreated, RA can cause serious joint damage relatively quickly, which is why early treatment is crucial. The good news is that modern treatments have revolutionized RA care.
Other Types Worth Knowing About:
Beyond OA and RA, there are other forms of arthritis worth mentioning. Gout happens when uric acid crystals build up in your joints usually your big toe and cause sudden, intense pain. It’s extremely uncomfortable but often treatable. Psoriatic arthritis occurs in people who have psoriasis, an autoimmune skin condition. Ankylosing spondylitis primarily affects the spine. Lupus can involve joint pain as part of its broader effects on the body.
The reason understanding these different types matters is that treatment varies significantly. What works great for osteoarthritis might not help with rheumatoid arthritis. That’s why getting the right diagnosis from a healthcare provider is so important it determines what approach will actually help you.
What Causes Arthritis The Risk Factors You Should Know About
Age: The One Risk Factor You Can’t Change:
Let’s be honest getting older increases your arthritis risk. Your cartilage doesn’t repair itself as efficiently, your body produces less synovial fluid, and years of movement add up. But here’s the important part: getting older doesn’t guarantee you’ll get arthritis. Some people live their whole lives without significant arthritis, while others develop it earlier.
This is where genetics come in. If your parents or grandparents had arthritis, you’re at higher risk. It’s not destiny, but it’s a factor worth acknowledging. You can’t change your age or your family history, but you can change other factors.
Lifestyle and Activity Choices:
The relationship between activity and arthritis is nuanced. Sedentary lifestyles contribute to weakness, poor joint stability, and weight gain all risk factors for arthritis. But excessive stress on joints from high-impact activities or repetitive strain can also increase arthritis risk. It’s about balance.
Weight matters too, and this is one area where you have control. Every pound of extra weight puts stress on your joints, especially weight-bearing joints like your knees and hips. Interestingly, losing even 5 to 10 percent of your body weight can significantly reduce joint pain and stress on your joints.
Previous Injuries and Joint Trauma:
If you’ve injured a joint through sports, accidents, or anything else that joint is more vulnerable to arthritis. This doesn’t mean you shouldn’t be active or take reasonable risks, but it does mean paying extra attention to those previously injured joints. Protecting them and keeping the surrounding muscles strong can help prevent or delay arthritis.
Occupational and Repetitive Stress:
Certain jobs put you at higher arthritis risk. People who spend years doing repetitive motions whether that’s typing, assembly work, or manual labor sometimes develop arthritis in those heavily used joints. This doesn’t mean you should avoid work, but it might mean paying attention to ergonomics and taking breaks to give your joints recovery time.
Autoimmune Factors:
For conditions like rheumatoid arthritis, the cause is your immune system misfiring. Genetic predisposition plays a huge role, but researchers believe environmental triggers things like infections or certain exposures might flip the switch. This is still being studied, but it highlights that autoimmune arthritis is different from the wear-and-tear variety.
| Factor | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
| Primary Cause | Wear and tear of cartilage | Immune system attacking joint linings |
| Onset | Gradual, develops over years | Often sudden, can develop quickly |
| Age of Onset | Usually over 50, but can occur younger | Any age, but often 30-60 |
| Affected Joints | Usually weight-bearing joints or hands | Multiple joints, often symmetrical |
| Morning Stiffness | Short-lived, improves with movement | Often lasts over 30 minutes |
| Systemic Symptoms | Mainly joint-related | Fatigue, fever, general malaise common |
| Progression Speed | Slow to moderate | Can be rapid without treatment |
| Treatment Approach | Pain management, physical therapy | Immune-suppressing medications crucial |
| Damage Reversibility | Cartilage damage is permanent | Can be stopped with early treatment |
Treatment Options: What Actually Works
Pain Management Beyond Just Popping Pills:
When arthritis pain hits, people often reach for over-the-counter pain relievers. That’s not wrong, but it’s just the beginning. Ibuprofen and similar nonsteroidal anti-inflammatory drugs (NSAIDs) reduce both pain and inflammation, which can really help. Acetaminophen handles pain but doesn’t reduce inflammation.
These work best for mild to moderate pain, and they’re meant for short-term or occasional use. Using them constantly can cause stomach issues and other problems. So while they have a place in your arthritis toolkit, they shouldn’t be your only tool. Think of them as first aid, not the cure.
Physical Therapy and Exercise: The Underrated Powerhouse:
Want to know a secret that seems too simple to work? Moving actually helps arthritis. I know, it sounds backwards when movement causes pain, but here’s what happens. Exercise keeps your joints mobile, strengthens the muscles that support those joints, and improves your overall function. Physical therapy specifically targets the joints causing problems, using exercises designed to improve movement without causing damage.
The key is doing the right exercises for your specific arthritis type. High-impact activities might hurt, but low-impact options like swimming, walking, or cycling are usually great. A physical therapist can design a program specifically for you, accounting for which joints are affected and what your limitations are.
Studies consistently show that people who exercise regularly have better outcomes with arthritis. They have less pain, better mobility, and slower progression. It’s not magic it’s just how your body works. Movement keeps everything functioning better.
Medications Disease-Modifying Options:
For rheumatoid arthritis and other autoimmune types, medications that modify the disease process have been game-changers. These drugs work by calming down your overactive immune system. Methotrexate, biologic medications, and other disease-modifying antirheumatic drugs (DMARDs) can slow or even stop joint damage.
These aren’t pain relievers they’re system-changers. They work on the underlying problem rather than just treating symptoms. The tricky part is that they usually take weeks or months to work, and they need to be carefully monitored. But if you have RA, these medications can mean the difference between progressive joint damage and a stable condition.
For osteoarthritis, there’s no disease-modifying medication because the underlying process is different. Treatment focuses on managing symptoms and slowing progression.
Injections and Targeted Treatments:
Corticosteroid injections directly into affected joints can provide significant relief, especially when one or two joints are particularly problematic. These injections reduce inflammation right where you need it, and they work relatively quickly. The downside is that the effect isn’t permanent, usually lasting weeks to months.
Hyaluronic acid injections are another option, especially for knee arthritis. These injections add lubrication to the joint, similar to what your body should be producing naturally. They take several weeks to work, but many people report significant improvement.
Lifestyle Modifications The Stuff That Actually Matters:
Here’s what healthcare providers don’t always emphasize enough: your daily choices matter enormously. Weight management, staying active, protecting your joints from unnecessary stress, maintaining good posture, and using proper ergonomics all reduce arthritis pain and slow progression.
Cold and heat both have roles. Heat relaxes muscles and improves blood flow, great for stiffness. Cold reduces swelling and numbs pain, better for acute inflammation. Many people use heat in the morning to loosen up stiff joints and cold after activity to reduce any resulting inflammation.
Joint protection techniques matter too. Using assistive devices for daily tasks things like jar openers, ergonomic keyboards, or canes isn’t giving up; it’s being smart about preserving your joints. The less stress you put on damaged joints, the longer they’ll function for you.
Emerging Treatments and Research:
Scientists are constantly working on new arthritis treatments. Regenerative medicine approaches like stem cell therapy and platelet-rich plasma injections are showing promise, though they’re not yet standard treatments. Gene therapy for rheumatoid arthritis is being studied. These are exciting possibilities, but they’re not replacements for proven treatments yet.
Living Better with Arthritis Practical Strategies That Work
Creating a Joint-Friendly Home Environment:
You don’t need to overhaul your entire home, but some thoughtful changes make life significantly easier. Grab bars in bathrooms prevent falls and reduce stress on joints. A shower stool lets you sit while bathing, taking pressure off knees and hips. Lever-style door handles are easier to use than round doorknobs when your hands are painful.
Storage matters too. Keep frequently used items at easy-to-reach heights. Reaching overhead or bending repeatedly to low shelves aggravates many people’s arthritis. Simple organization makes huge differences in daily pain levels.
Pacing and Activity Management:
People with arthritis often adopt an all-or-nothing approach: either they’re sedentary because moving hurts, or they push hard and then suffer for days. Neither extreme works. Instead, pacing spreading activity throughout the day and taking breaks helps you accomplish more without flaring up pain.
This is called the “spoon theory” in chronic illness communities. Everyone has a limited amount of energy (spoons). Arthritis costs extra spoons, so you prioritize what’s most important and pace accordingly. Some days you’ll have more spoons; other days fewer. That’s normal.
Managing Flare Ups When Arthritis Gets Worse:
Arthritis symptoms aren’t always consistent. Sometimes you have days or weeks where everything hurts more and movement is more limited. These are flare-ups, and they’re frustrating. They usually pass, but you need strategies to get through them.
During flare-ups, reduce activity, use ice or heat as appropriate, and consider temporarily increasing pain management. If you have medications for flare management, this might be when you use them. Most importantly, recognize that flare-ups are temporary. They feel permanent when you’re in one, but they pass.
| Treatment Method: | Onset Time: | Effectiveness: | Duration: | Side Effects: |
| NSAIDs (Ibuprofen/Naproxen) | Hours | Moderate | Hours to days | GI upset, possible |
| Physical Therapy | Weeks | High with consistency | Ongoing benefit | Minimal |
| Corticosteroid Injections | Days | High (localized) | Weeks to months | Low for short term |
| DMARDs (Rheumatoid Arthritis) | Weeks to months | Very high (stops progression) | Ongoing | Varies, requires monitoring |
| Weight Loss (5-10%) | Gradual | Moderate to high | Ongoing | Minimal |
| Heat/Cold Therapy | Minutes | Mild to moderate | Hours | None |
| Biologic Medications | Weeks | Very high | Ongoing | Requires monitoring |
The arthritis landscape has changed dramatically over the past few decades. Twenty years ago, people with rheumatoid arthritis often faced progressive joint destruction despite treatment. Now, many people achieve remission and don’t develop significant joint damage. That’s huge. It shows that ongoing research and medication advances really do improve lives.
For osteoarthritis, the picture isn’t as dramatic but it’s still improving. Better physical therapy approaches, regenerative medicine research, and a stronger emphasis on early intervention mean people are managing OA better than ever. We’re learning that it’s not inevitable that arthritis equals disability.